Revenue Cycle Management
Agisol partners with healthcare organizations to speed up reimbursements, close gaps for denials,
stop revenue leakages, reduce costs, and improve patient experiences with disruptive automation
technologies.
PATIENT SCHEDULING AND APPOINTMENT
Agisol helps patients schedule appointments without long hold times, in turn helping providers manage appointments smoothly. We communicate directly with providers and patients through a messaging system, call patients to inform them of their appointments and confirmations, and send automated reminders to both patients and providers.
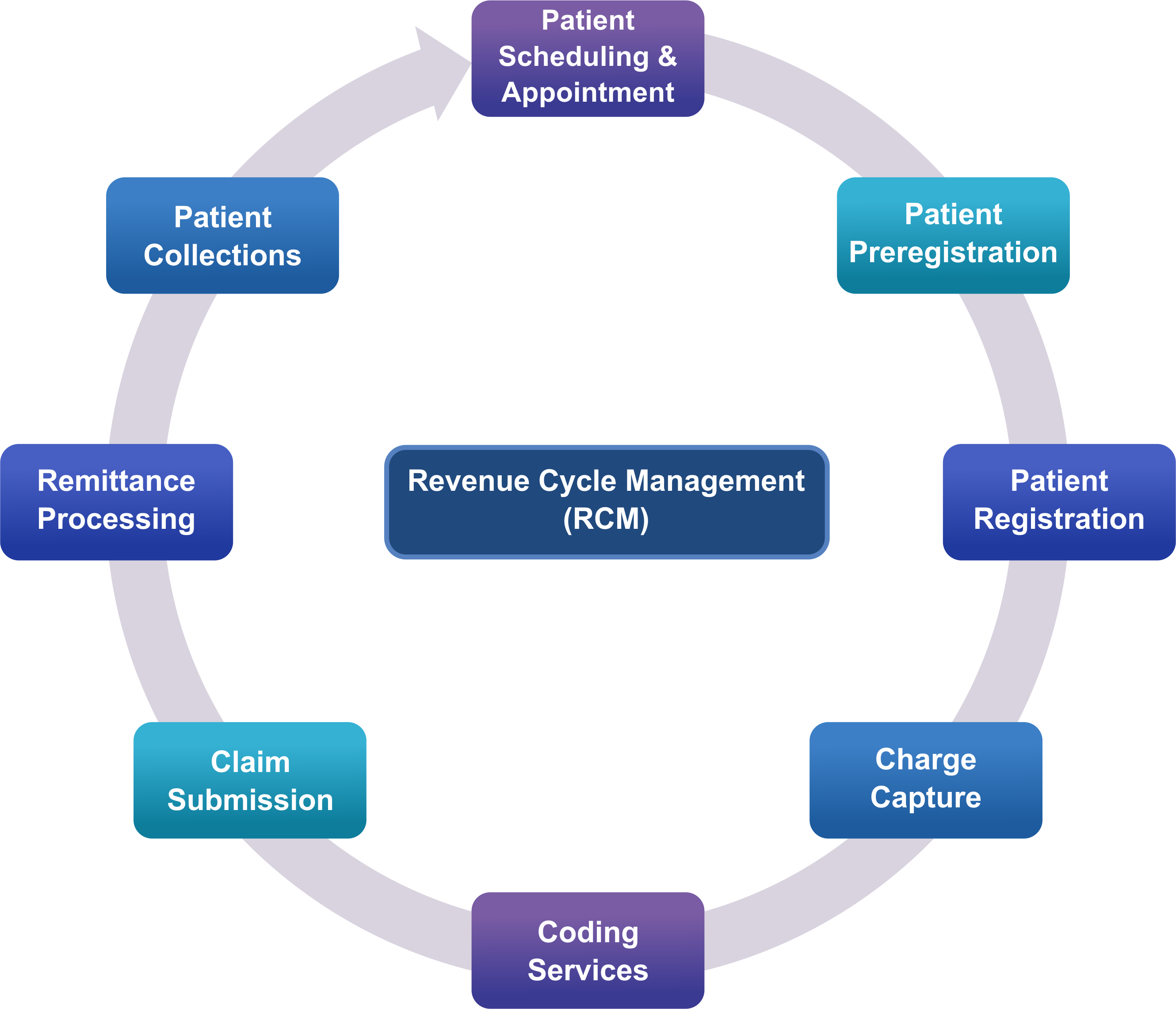
Patient Preregistration:
Agisol helps medical practices capture important patient demographics, insurance information, and
eligibility through a clearing house. This helps the provider’s practice management system know about the patient’s coverage, deductibles, co-insurance, co-payments, and referrals. Preregistration is the first step and determines the financials for the provider, making it a key process for a strong start to the revenue cycle.
Patient Registration
After preregistration, the registration process becomes easier to obtain 100% of the patient’s information. During registration, the provider ensures that the patient’s demographics, guarantors, and insurance information are accurate and become a record for future references. At this stage, co-payments are collected and referrals and authorizations for treatments are processed. All financial forms are signed and insurance benefits are assigned. Agisol’s expert team
thoroughly handles all of the above, ensuring that all documents are ready in case of an audit and the practice can easily avoid all financial risks.
Charge Capture
Agisol’s expert team captures charges through two methods: manually or through an automated process, which includes ancillary services and coding services.
Coding Services
Agisol’s coding team enables healthcare providers to prevent revenue leakage by ensuring accurate coding, reducing discharges that are not fully billed. Based on the findings from our internal audit team, we drive clinical documentation initiatives and collaborate with providers to reduce denials.
Claim Submission
After capturing charges, Agisol’s team works on submitting claims to insurance carriers. The revenue cycle team checks for any charge issues, ensures accurate CPT and diagnosis codes, and scrubs claims of errors to ensure clean and fast processing. Agisol sends claims from the provider’s practice to a clearinghouse, acting as a mailroom and
sending them to different insurance payers. Transmission reports are generated, and any rejections are reviewed and immediately fixed to speed up payment.
Remittance Processing
Explanation of benefits in the remittances help the Agisol team to understand the details of the payments made to the providers for their services. Allowables are determined in this process according to the provider’s contract with insurance carriers for the services provided.
The Agisol team verifies any shortfalls in the remittances that are usually neglected by the provider’s team due to a lack of time to go through every EOB. The Agisol team appeals for such errors to get back the partial payments. This process includes reviewing the fee schedules on an annual basis to ensure that the fees are adjusted in rates, contracts, and allowables. Write-offs and contractual write-offs cannot be prevented as they involve the actual contracted rates with payers. Agisol looks for points that can be avoided in the remittance process which can affect the RCM and helps the providers avoid unnecessary reprocessing. The Agisol A/R report regenerates reports bucket-wise for a period of time. The Agisol team is capable and cross-trained for different carriers and aging reports, different practice managements, Medicare, Medicaid, and appeals. Denial management is critical to maintaining a healthy cash flow. The Agisol team focuses mainly on the root cause and denial prevention.
Patient Collections
Agisol’s team sends out monthly statements for patient collections to remind patients of their
deductibles and co-payments.
